Summary
In June 2021, the World Health Organisation commissioned the VCP to examine public perceptions and uptake of the COVID-19 vaccine in 13 countries across the Asia-Pacific.
At this stage of the pandemic, hopes for a return to a sense of ‘normality’ rested on the development of a vaccine that people across the world were willing to accept. It was therefore vital to understand public attitudes to Covid-19 vaccination across the Asia-Pacific.
The aim of the study was to investigate public knowledge and perceptions of both the COVID-19 pandemic itself and COVID-19 vaccine acceptance among adults (aged 18 years and above), in order to identify knowledge gaps, beliefs and attitudes that can help inform the World Health Organisation (WHO) as well as other immunisation stakeholders in their strategies for supporting the roll-out of Covid-19 vaccines in the region.
In July 2022, the The Vaccine Confidence Project (VCP) published an analysis examining the factors associated with vaccine confidence across the Western Pacific by using 10,581 responses from the 2021 (Wave 1) data collection.
A subsequent report has also been developed using data from 7,908 responses from a secondary wave of quantitative data collection, conducted between May and June 2022.
Methodology
Both the initial and secondary wave of fieldwork was carried out by ORB International using telephone (CATI – computer assisted telephone interviewing) and online approaches in different countries, with 500-1,000 interviews in each country.
To identify drivers of vaccine hesitancy across the region, the VCP analysed the dataset by:
- Examining the political/sociodemographic factors associated with low vaccine acceptance by using descriptive statistics and regression techniques.
- Using Latent Class Analysis (LCA) to capture smaller risk groups that are less likely to accept COVID-19 vaccines.
Findings
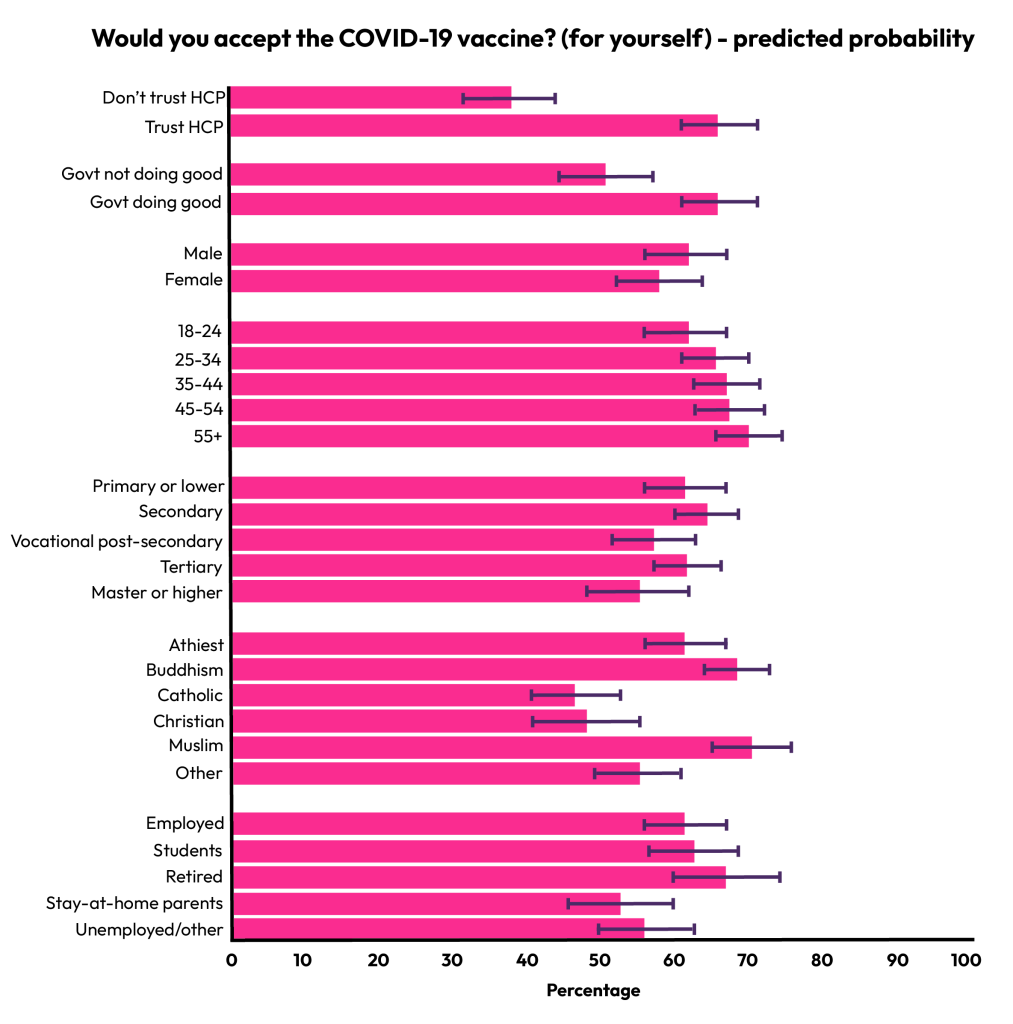
The analysis of the Wave 1 data revealed that trust in local health care providers and perception of the government doing good were the strongest determinants of vaccine acceptance.
A further four risk groups with lower vaccine acceptance (for self and for others) were identified among six latent class subgroups (in bold below):
- Group 1. COVID as Flu (64% for self, 65% for others)
- Group 2. The Elderly (73% for yourself, 74% for others)
- Group 3. Distrust in Authorities (52% for self, 65% for others)
- Group 4. Stay-at-home Mothers (55% for self, 65% for others)
- Group 5. College Students (59% for self, 69% for others)
- Group 6. General Working Population (66% for yourself, 73% for others)
We found that countries in the Western Pacific could be categorised into four categories depending on their composition of vaccine-reluctant respondents:
Category 1. Papua New Guinea, Solomon Islands, Tonga, and Vanuatu: In these countries, low vaccine acceptance was driven by distrust in authorities and low risk perception of COVID-19. Resolving vaccine hesitancy may be more complicated in these countries due to multiple causes. These countries may need public messages or campaigns to raise awareness of the risk of COVID-19, in addition to strategies for building trust in government and health authorities.
Category 2. Fiji, Japan, and Philippines: Stay-at-home mothers took a large portion of vaccine-reluctant people. Studies find that social media information has a growing impact on the vaccination choices of mothers and women of childbearing age. Therefore, measures to improve understanding of the safety of vaccines among women and mothers and social media management would be beneficial for these countries.
Category 3. Lao PDR, Malaysia, the Republic of Korea: Low vaccine acceptance was driven by distrust in authorities. Efforts to understand the root cause that undermines trust in government and medical experts and vaccine campaigns that rebuild trust are necessary in these countries.
Category 4. Cambodia, Mongolia, and Viet Nam: There are no distinct risk groups in these countries. These countries had a high rate of vaccine acceptance, and the vaccination rate was also sharply growing over the period of this survey. Therefore, for these countries, it would make sense to maintain the current status of public trust in government and the medical establishment and keep providing consistent public messages of public health recommendations while continuously monitoring the possible risk factors of vaccine hesitancy.
The LCA results in the Wave 2 report largely replicated the subgroups in the VCP’s Wave 1 report, highlighting two risk groups with lower booster vaccine uptake (in bold) among five subgroups: stay-at-home mothers and distrusters of health care providers.
- Group 1. College students (35%)**
- Group 2. Stay-at-home mothers (44%)
- Group 3. The elderly (68%)
- Group 4. Distrusters of health care providers (44%)
- Group 5. General Working Population (56%)
* Booster vaccination rate in parentheses
** In many countries, this group was not prioritised in the distribution of booster vaccines until the second wave data collection period.
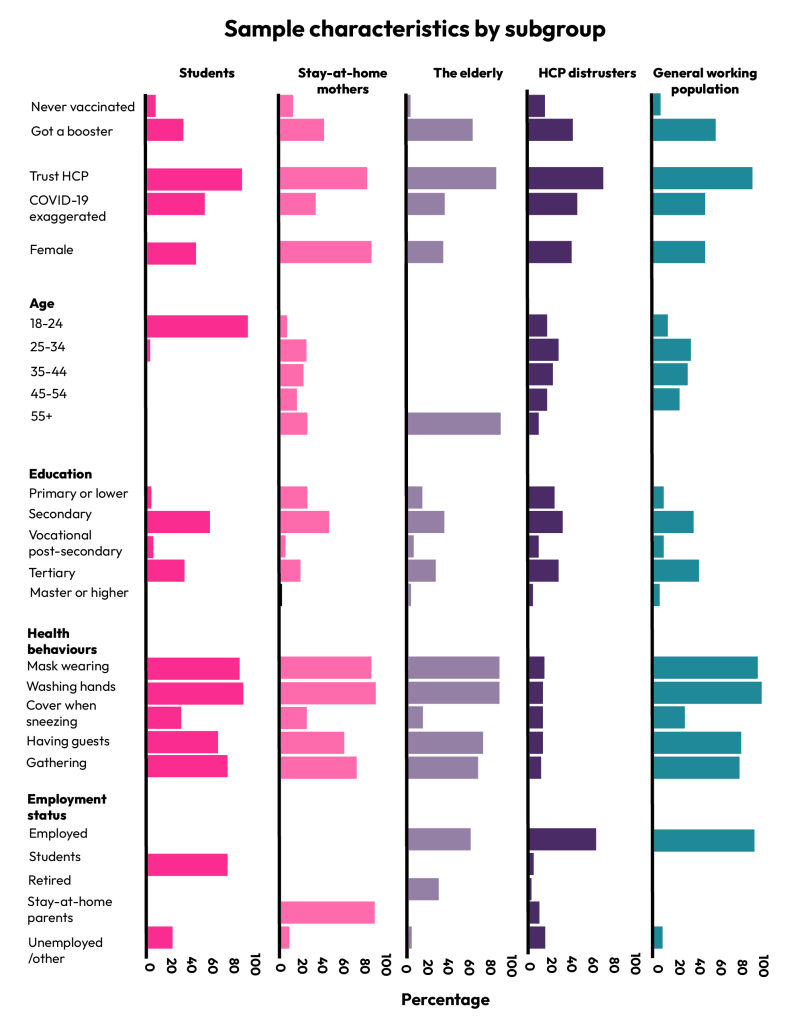
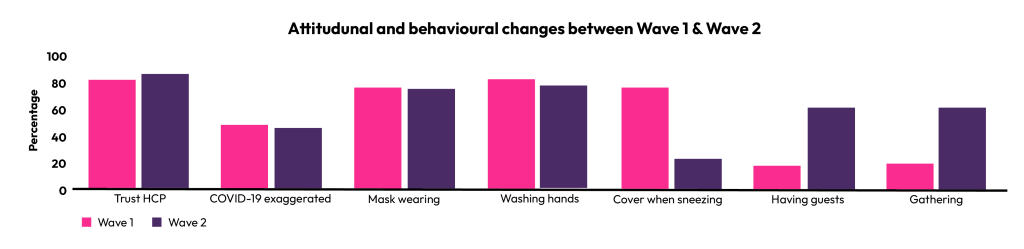
Between Wave 1 and Wave 2, public trust in local health care providers and the risk perception of COVID-19 remained at a similar level across the Western Pacific. People also wore masks and washed their hands at a similarly high rate.
However, there were substantial changes in adherence to other public health recommendations. The percentage of people answering that they cover their mouth and nose when sneezing dropped from 77.1% to 24.1%, and the percentages of people who said they had engaged in the two types of social mixing– having guests and gathering – increased from 18.6% and 19.7% to 61.5% and 62.1%, respectively.